Biography
Training
- 2014 HDR, Faculty of Medicine Pitié Salpêtrière, specialties Neurosciences.
- 2001 Doctorate in Neurosciences, Paris XII.
- 1996 Master's degree in Cellular Biology and Physiology, Paris XII.
Functions and posts held
Since 2011 Researcher, CR1, Paris Brain Institute, INSERM 1127, Paris, France. Role of neuroinflammation in remyelination.
2004-2011 Post-doctoral collaborator in the laboratory of Dr Baron Van Evercooren, CRICM, INSERM U975 Paris, France. Contribution of peripheral nervous system cells to central nervous system repair: molecular and cellular analysis.
2001-2004 Post-doctoral associate in the laboratory of Dr. Harrison, Department of Pharmacology, University of Florida, Florida, USA. Development of a chemokine antagonist using a viral protein vMIP II. Identification of novel genes involved in peripheral nervous system regeneration.
1998-2001 Doctor in central nervous system Dr. Jesus Benavides Department of Sanofi-Synthélabo, Bagneux, France. Role of Fractalkine in the development of inflammation in the central nervous system.
Scientific areas
Neuroinflammation/Rehabilitation/ Multiple Sclerosis
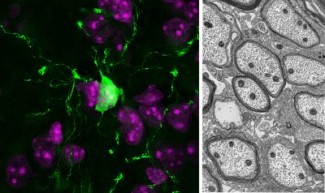
Multiple sclerosis (MS) is an inflammatory and neurodegenerative disease in which the infiltration of immune cells into the central nervous system (CNS) results in the destruction of myelin. But immune cells can also participate in the myelin repair process by orchestrating the activation, recruitment and differentiation of new myelin-forming cells. Our group aims to describe how defects in macrophages and lymphocytes contribute to MS pathology.
To understand the role of lymphocytes in remyelination, we developed a humanized mouse model of remyelination by grafting lymphocytes from healthy controls or MS patients into a demyelinated nude mouse lesion. We replicated the heterogeneity of patient remyelination in this model demonstrating that lymphocytes from some MS patients interfere with remyelination (El Behi , Sanson et al, 2017). We also noted that the modulatory effects of remyelination of patient lymphocytes are mediated by macrophage activation.
The role of macrophages has mainly been described in terms of animal models and estimates based on postmortem tissues. By studying macrophages derived from patients' monocytes, we are trying to elucidate how their innate properties and response to activation stimuli are linked to disease, both at the group level and at the individual patient level. Our results indicate that macrophages of MS patients exhibit functional and molecular dysfunctions prior to any exposure to lesions. In particular, monocytes from MS patients show preferential differentiation to pro-inflammatory CD16+ macrophages, exaggerated inflammatory response even in the absence of pro-inflammatory stimuli, and blockade of mitochondrial metabolism. All these characteristics are traits reminiscent of trained immunity (Fransson et al., submitted in 2021).
We propose to complement these observations and to precisely define the molecular mechanism leading to the over-activation of macrophages in MS patients by studying the epigenetic regulation (histone modification, regulation of long noncoding RNAs) of macrophages in MS patients.
We have also developed a method for identifying key regulators in networks of several altered genes. This was done in terms of a predefined network of genetic interactions. By testing a pro-inflammatory network for the possibility of controlling genes that are deregulated in MS, we have identified biologically and pathologically relevant genes as key regulators, supporting the framework of the method (Bassignana et al, Network neuroscience in review https://arxiv.org/abs/2003.08913).
Our preliminary results show that macrophages contribute to an inflammatory environment and that the heterogeneity of patients, both lymphocytes and macrophages, has an impact on this contribution. Further research using these and similar models could be useful both in developing new treatments and in predicting effects for individual patients.
Main publications
- Dysregulated functional and metabolic response in multiple sclerosis patient macrophages correlate with a more inflammatory state, reminiscent of trained immunity. (2021) J. Fransson, C. Bachelin, F. Deknuydt, F. Ichou, L. Guillot-Noël, M. Ponnaiah, A. Gloaguen, E. Maillart, B. Stankoff, A. Tenenhaus, F. Mochel, B. Fontaine, C. Louapre, V. Zujovic. BioaRCiv doi: https://doi.org/10.1101/2021.01.13.426327.
- Step-wise target controllability identifies dysregulated pathways of macrophage networks in multiple sclerosis. (2021) Giulia Bassignana, Jennifer Fransson, Vincent Henry, Olivier Colliot, Violetta Zujovic, Fabrizio De Vico Fallani. Network Neuroscience (in press). Advance publication. https://doi.org/10.1162/netn_a_00180.
- Activation of Macrophages by Lysophosphatidic Acid through the Lysophosphatydic Acid Receptor 1 as a Novel Mechanism in Multiple Sclerosis Pathogenesis. (2020) Fransson J, Gómez-Conde AI, Romero-Imbroda J, Fernández O, Leyva L, de Fonseca FR, Chun J, Louapre C, Van-Evercooren AB, Zujovic V, Estivill-Torrús G, García-Díaz B. Mol Neurobiol. doi: 10.1007/s12035-020-02130-x
- Adaptive human immunity drives remyelination in a mouse model of demyelination. (2017). El Behi M.#, Sanson C.#, Bachelin C., Guillot-Noël L., Fransson J., Stankoff B., Maillart E., Sarrazin N., Guillemot V., Abdi H., Cournu-Rebeix I., Fontaine B., Zujovic V. Brain. Apr 1;140(4):967-980
- Modulation of the Innate Immune Response by Human Neural Precursors Prevails over Oligodendrocyte Progenitor Remyelination to Rescue a Severe Model of Pelizaeus-Merzbacher Disease. (2016) Marteyn A, Sarrazin N, Yan J, Bachelin C, Deboux C, Santin MD, Gressens P, Zujovic V, Baron-Van Evercooren A. Stem Cells 34(4):984-96