Progressive supranuclear palsy (PSP), also known as Steele-Richardson-Olszewski Syndrome, is a rare neurodegenerative disease that affects between 5,000 and 10,000 people in France, with onset between the ages of 40 and 60. It accounts for 3–6% of all atypical Parkinsonian syndromes. The clinical picture for this condition is similar to that of Parkinson’s disease, but with specific clinical signs. These include an unstable posture, leading to involuntary falls backwards (retropulsions), neck muscle hypertonia (retrocollis), eye movement paralysis or disorders.
Biological mechanisms and causes of progressive supranuclear palsy
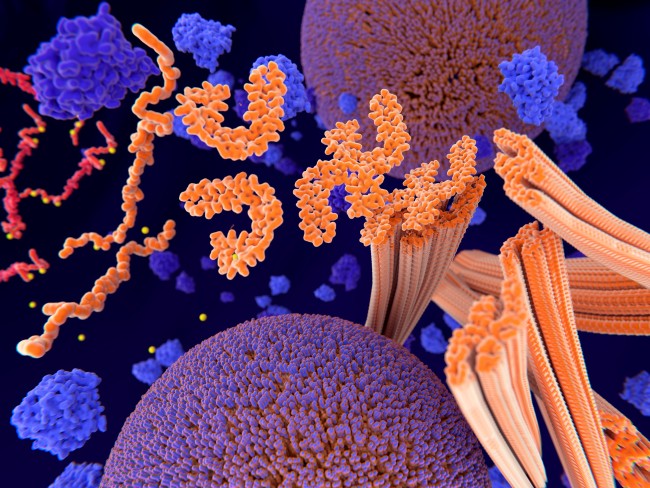
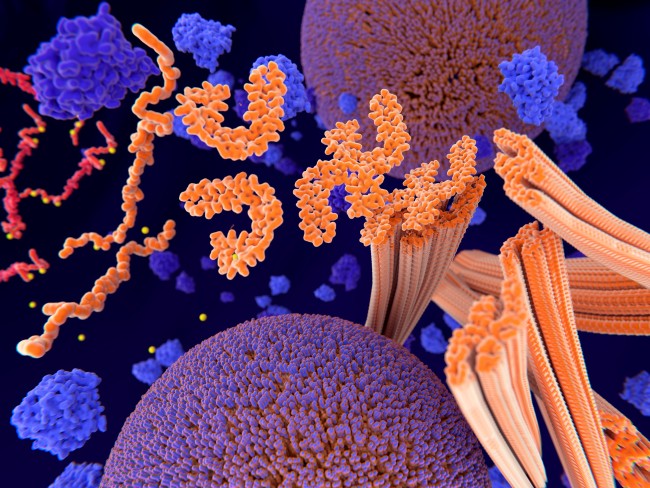
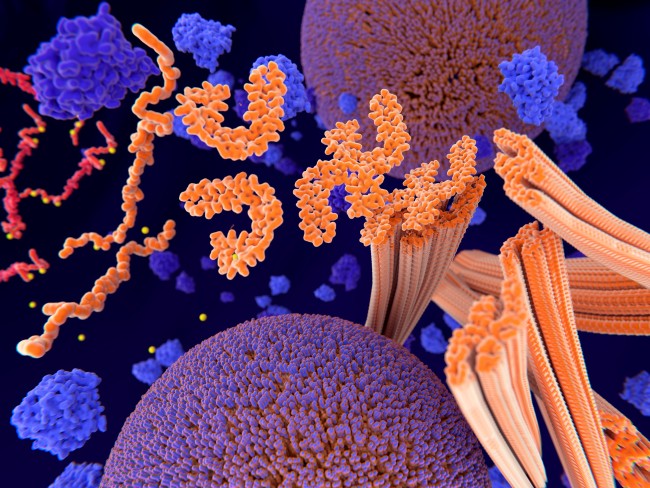
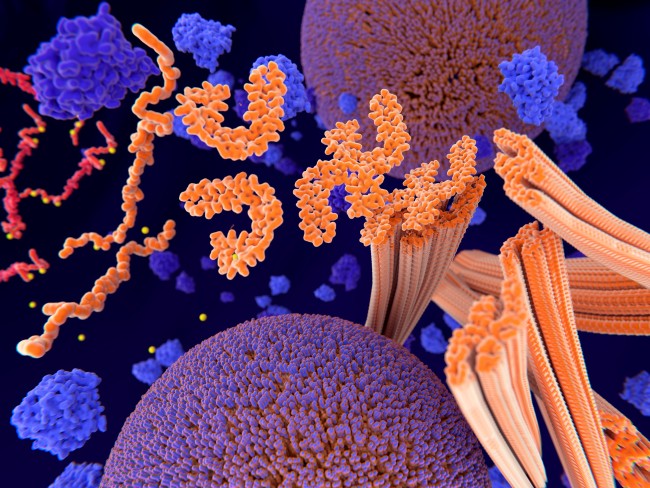
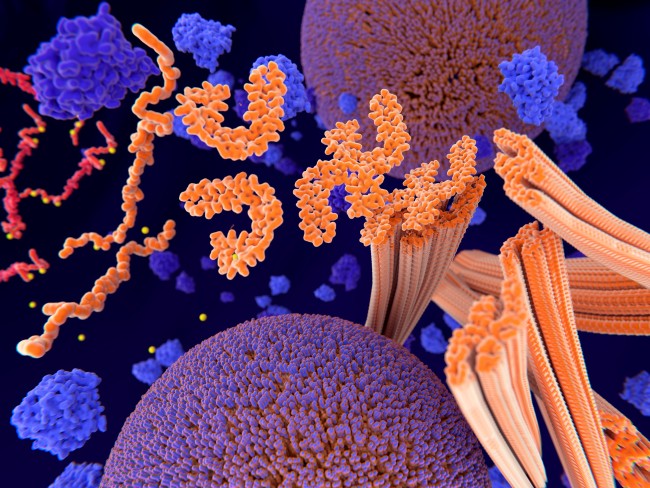
In progressive supranuclear palsy (PSP), there is an abnormal accumulation of a protein known as the tau protein in neurons, causing them to degenerate. PSP is described as tauopathy. The exact cause of PSP is still unknown. The hypothesis that PSP is a multifactorial disease has been put forward – a genetic predisposition combined with environmental influences is the likely cause of the condition, but it is not hereditary. In just a few tens of families worldwide, a mutation has been identified in a gene coding for a microtubule protein.
The neuronal death associated with the accumulation of the tau protein affects all regions of the brain, but has a greater impact on the basal ganglia and brain stem. The basal ganglia are brain structures that initiate and harmonise voluntary movements and control changes in posture. The brain stem regulates vital functions such as breathing, heart rate and swallowing.
Progressive supranuclear palsy symptoms and diagnosis
PSP has a combination of systems, ranging from motor symptoms like unstable posture and muscle stiffness to eye movement disorders and eyelid occlusion, as well as cognitive and behavioural symptoms such as an unstable mood, with the patient often presenting with involuntary crying or laughter. PSP is diagnosed based on neuropsychological tests, brain imaging through MRI and/or PET scans, and oculomotor screening to identify any eye movement disorders.
Treatment for progressive supranuclear palsy
Currently, there are no drug treatments that can cure PSP. However, certain treatments generally prescribed for Parkinson’s disease can alleviate some of the symptoms experienced by PSP patients at the condition's onset.
Treatment for PSP is symptomatic and multidisciplinary, and includes physiotherapy and speech therapy to help with progressive muscle stiffness, and to preserve joint flexibility for as long as possible, limiting the risk of falls.
In 2019, France’s agency for the safety of medicines and health products (Agence national de Sécurité du Médicament, ANSM) authorised the launch of a phase 2a clinical trial with the drug candidate AZP2006. This therapeutic trial is taking place at La Pitié Salpêtrière Hospital in Paris (AP-HP), under the direction of Professor Jean-Christophe Corvol, neurologist and researcher at Paris Brain Institute and at Lille teaching hospital (CHU), within Professor Defebvre’s department.
Support Paris Brain Institute
Did you like this content and did it answer the questions you were asking? Don't hesitate to support Paris Brain Institute.