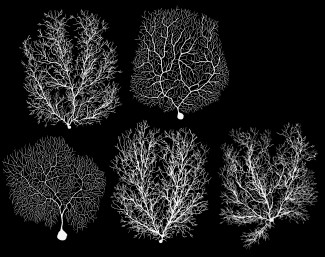
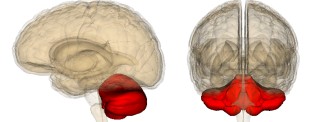
Depending on the nature of the ataxia, whether acquired or genetic, a variety of symptoms can be observed. Nevertheless, a large majority of patients have cerebellar symptoms, which are related to cerebellar dysfunction.
Symptoms of Ataxia
Symptoms related to coordination or cerebellar disorders may be of different types. A distinction is made between:
- Ataxia: Unstable, stumbling, walking with legs or bars apart to maintain balance.
- Dystopia: Loss of control of the amplitude of movements, slower and jerky gestures, impossibility of performing fine gestures such as writing.
- Dyarthria: Inable to articulate words correctly, speech is impaired with loss of control of voice amplitude and lip movements.
- The nystagmus: rapid, involuntary eye oscillations. The eyes move in all directions and slowly return to the original position.
Acquired ataxia
The symptoms of acquired ataxia are very heterogeneous and depend on the location and type of brain injury, which causes them, such as tumour, cyst, hematoma, inflammation.
Neurological disorders such as tremors, dementia, but also cardiac, skeletal and endocrine disorders can be observed in patients.
Diagnosis of acquired ataxia is made by clinical examination, medical imaging, oculomotor examinations or an electroencephalogram.
Treatments for acquired ataxia address the cause of the symptoms. Stopping alcohol use or decreasing drug doses in cases of toxic ataxia, cyst or tumour surgery and treatment of inflammation.
Genetically Induced Cerebellar Ataxia
Autosomally dominant ataxia
Individuals with these ataxia have the cerebellar symptoms, listed above, that indicate cerebellar damage.
There are four clinical tables:
Type 1: Cerebellar symptoms are accompanied by eye damage, with reduced eye movements that may lead to paralysis. Muscle stiffness (dystonia) or muscle loss (alyotrophy) may also occur, but sensitivity disorders may prevent the patient from being aware of the position of his or her body. In some very severe cases, an intellectual deficit can be observed.
Type 2: Cerebellar symptoms are associated with degeneration of retinal cells that may lead to loss of vision.
Type 3: the patient has only cerebellar disorders.
Type 4: a combination of cerebellar symptoms and epilepsy.
Diagnosis of these ataxies combines a clinical examination, brain imaging, a family study with the search for the genetic mutation.
To date, there is no cure for predominantly transmitted ataxia, but the treatment of symptoms by physiotherapy, occupational therapy, speech therapy and psychomotor rehabilitation makes it possible to reduce the disability.
Autosomal recessive ataxia
The ataxia of FRIEDREICH
Friedreich’s ataxia usually begins with cerebellar disorders such as walking disorders, instability, and then upper limb coordination disorders. As speech disorders (dysarthria) progress, swallowing, vision or hearing may occur.
Patients often have bone deformities in the spine or plantar wall. In childhood, heart disease may occur 4 to 5 years after the onset of the disease and diabetes occurs in 10 to 20% of cases.
Diagnosis is based on age criteria, with this pathology generally beginning between the ages of 7 and 14, clinical symptoms and very often abnormalities on the electromyogram (recording of electrical signals from the muscles) and on the cardiac ultrasound. Identification of a genetic mutation confirms the diagnosis.
A treatment for this ataxia is being evaluated specifically to decrease cardiac involvement. As with other ataxia therapies, physiotherapy, occupational therapy, speech therapy and psychomotor rehabilitation allow the patient to maintain a quality of life for longer.
Telangiectatic ataxia
The symptoms of telangiectatic ataxia appear around the age of 2 years are numerous and may involve the nervous system, the skin, the immune system.
In addition to the cerebellar symptoms described above, there is dilatation of peripheral vessels, sometimes signs of premature aging (white hair, finer skin) and increased susceptibility to infection due to dysfunction of the immune system.
In addition to the clinical examination made difficult by the age of the affected children, the diagnosis is based on biological criteria such as the level of certain proteins or antibodies and the identification of the genetic mutation.