Epilepsy can begin at any age. Because seizures are intermittent and unpredictable, they are a threat that is constantly hanging over patients, massively impacting their quality of life.
Treatments for epilepsy
The right treatments for epilepsy depend on the type of epilepsy (focal or generalized) and its cause (injury, genetics, etc.).
Treatment must be holistic, aiming on the one hand to stop seizures from happening or at least alleviate them, and on the other to eliminate or correct their causes. It must also identify and address the consequences of the disease on the patient’s life, for example any learning problems or depression.
Anti-epileptic therapies
Anti-epileptic medication applies different mechanisms to try to prevent seizures from recurring:
- by stabilizing neuron membranes by regulating the opening and closing of ion channels, especially channels permeable to sodium, preventing excessive propagation of neuronal discharges.
- by blocking excessive stimulation of receptors that agitate neurons (such as glutamate receptors)
- by activating receptors that inhibit neurons (such as GABA receptors)
- by modulating the release of synaptic vesicles.
The neurologist will choose from these treatments according to the type of seizure (some medication may be ineffective in absence seizures or myoclonic seizures), and individual patient (each treatment has side effects, so the choice will depend on the patient’s age, gender and any other conditions).
In 30% of patients, anti-epileptic drugs are ineffective. This means that identifying new anti-seizure mechanisms, and therefore developing new medicines, is essential. The epilepsy team at Salpêtrière hospital, in coordination with the Clinical Research Center at Paris Brain Institute, led by Dr Céline Louapre and Professor Jean-Christophe Corvol, focuses on early evaluation of new anti-epileptic drugs as part of therapeutic trials. This enables some patients to benefit from new medication before it comes onto the market.
Surgery for epilepsy
For drug-resistant focal epilepsy, removal of the brain area causing the seizures can be considered.
To target the brain area responsible for the seizures, the epileptogenic focus, clinicians and researchers at Paris Brain Institute use a range of technologies at a technical facility that is unique to the Paris Region. The pre-surgery assessment requires:
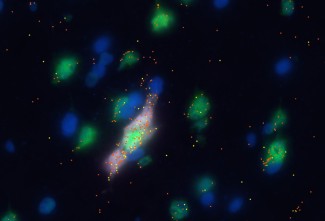
- Surface, and sometimes intracerebral, electroencephalography (EEG). These continuous recordings are taken 24 hours a day, 7 days a week, over a 2-3-week period at the epilepsy unit to monitor several seizures.
- Positron emission tomography (PET), carried out at the nuclear medicine department, identifies the brain areas that are not taking up glucose effectively, and which are therefore implicated in the epileptogenic focus.
- During a seizure, a SPECT scan visualizes the brain region activated by a seizure: this detects an increase in localized blood flow in the brain, linked to the increased energy needs of neurons recruited by the seizure.
- Through functional magnetic resonance imaging (fMRI), performed in the neuroradiology department, it can be assessed whether the brain area identified as causing the seizures can be operated on. If the area concerned is still functional – if it activates during certain exercises – surgery is rejected as an option.
When the exact brain region causing the epilepsy has been pinpointed using this complex technique, neurosurgical intervention is proposed: a resection of the epileptogenic focus at the neurosurgery department by Dr Bertrand Mathon enables full recovery in 50-80% of patients.
Other neurosurgical approaches, such as vagus nerve stimulation, may be proposed. The principle behind these approaches is chronic neuromodulation of the brain, to reduce the frequency and severity of seizures.
New techniques are being evaluated, including laser treatment of the epileptogenic region when conventional surgery is not an option.