Unlike classic epileptic seizures that last only a few seconds or minutes, "status epilepticus" refers to a state of neuronal hyperactivity in the cerebral cortex that persists for several hours or days. When this condition occurs without a readily identifiable cause in people with no previous neurological history, it is called New-Onset Refractory Status Epilepticus, or NORSE. This dreaded event exposes patients' brains to irreversible damage. Aurélie Hanin and Vincent Navarro at Paris Brain Institute, in collaboration with Lawrence Hirsch's team at Yale University, are investigating the pathophysiological mechanisms underlying these seizures to improve care management. In a new study published in the journal Annals of Neurology, the researchers show a disturbance of innate immunity in NORSE patients, characterized by the elevation of pro-inflammatory markers whose intensity is correlated with short and long-term prognosis.
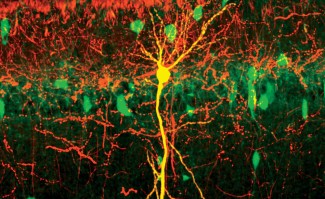
A rare and nevertheless formidable event in the landscape of epilepsies, New-Onset Refractory Status Epilepticus (NORSE) is a form of prolonged seizure in which the neurons of the epileptic focus endure a continuous discharge of neurotransmitters. It is a medical emergency requiring intensive care management. Indeed, it can cause significant long-term neurological sequelae and is associated with an average mortality rate of 12% in children and 16 to 27% in adults. NORSE can occur in response to an infection or tumor development. However, its origin remains unknown in half of the affected patients despite extensive clinical and biological examinations.
Currently, there is no consensus on the best therapeutic options for patient care. Understanding the pathophysiological mechanisms in NORSE is crucial to intervene early with the most appropriate treatment, hoping to prevent neuronal damage related to status epilepticus. At the moment, patients are empirically treated with immunotherapies to reduce inflammation. But this recommendation is not based on solid scientific evidence.
The first-ever large-scale study on NORSE
Identifying prognostic markers for the disease proved difficult because NORSE is rare and highly heterogeneous. To overcome this lack of data, Aurélie Hanin, a postdoctoral fellow, together with Vincent Navarro's team at the Brain Institute and Lawrence Hirsch's team at Yale University, recruited a cohort of 61 NORSE patients hospitalized in the United States, Canada, and La Pitié-Salpêtrière Hospital (AP-HP). Among them, 51 had cryptogenic NORSE, in which the cause of status epilepticus was not found.
The researchers assessed the patient’s clinical status right after they had been discharged from ICU, then after 12 months, and looked for inflammatory markers in the blood and cerebrospinal fluid. The same data was collected on a cohort of 37 patients with status epilepticus of known cause and 52 control patients.
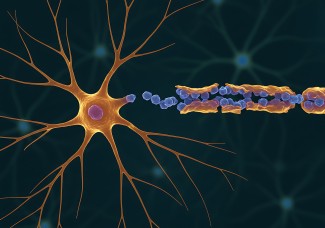
Our results show that the concentration of several cytokines – small proteins that attract inflammation cells – was higher in patients with status epilepticus than controls. Moreover, in subjects with an unknown cause of NORSE, the increase in cytokines related to innate immunity – CXCL-8/IL-8, CCL2, and MIP-1α – was correlated with poor short-term and long-term prognosis.
Perspectives for patient care
These results suggest that an innate immunity disturbance is involved in the onset of NORSE and its long-term consequences. They also confirm the interest in anti-inflammatory therapeutic strategies targeting one or more cytokines in these patients.
In the long run, quantifying and analyzing cytokines upon arrival in the ICU could give us a better understanding of the inflammatory state of NORSE patients and provide essential information support for the choice of specific immunomodulatory treatments. One of this study's major challenges was determining whether the increase in cytokines resulted from prolonged epileptic seizures or was directly related to a specific immune abnormality in NORSE. Now, we know that the latter hypothesis is more likely.
Further research will confirm that cytokines are promising biomarkers for NORSE – both for establishing the diagnosis, monitoring the patient's condition, and estimating neurological recovery capabilities after intensive care.
Funding
- Daniel Raymond Wong Neurology Research Fund (NORSE Institute, Yale)
- NORSE/FIRES Research Fund (Yale)
- Association Paratonnerre
- Fondation Assistance Publique des Hôpitaux de Paris (EPIRES – Marie Laure Merchandising)
- Institut Servier
- Philippe Foundation
Sources
Hanin, A et al., Cytokines in New-Onset Refractory Status Epilepticus Predict Outcomes, Annals of Neurology, 2023. 10.1002/ana.26627