Researchers from Inserm, CNRS, Sorbonne University and clinicians from the AP-HP and at Paris Brain Institute identified one of the mechanisms explaining ketamine effect as an antidepressant. Ketamine, usually used as an anesthetic, was administered to patients with severe resistant depression. This treatment led patients to present an increased ability to overcome their negative beliefs about themselves and the world when researchers presented them positive information. These results, published in JAMA Psychiatry, open new therapeutic avenues for the management of antidepressant-resistant mood disorders.
Depression is the most common psychiatric disorder: it is estimated that 5 to 15% of the French population will experience a major depressive episode during their lifetime. All age groups and all social backgrounds are affected.
The disease is characterized by sadness and loss of hedonic feelings that positive events do not improve. Depressed patients progressively develop negative beliefs about themselves, the world, and the future, that may develop into suicidal thoughts. These negative beliefs remain even when the patient receives positive information.
About one-third of people with depression do not respond to the most prescribed antidepressants, leading to a diagnosis of treatment-resistant depression (TRD). For these people, finding new and effective therapies is a priority.
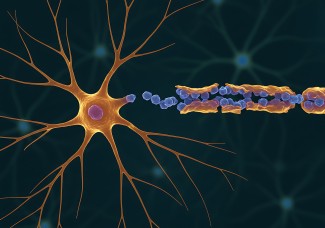
Ketamine, a commonly used anesthetic, has been shown to influence resistant depression. While conventional antidepressant treatments take time to be efficient (on average three weeks), ketamine has a rapid antidepressant effect, only a few hours after administration. The mechanisms associated with this fast-acting antidepressant effect are still unknown.
To identify these mechanisms, Dr. Hugo Bottemanne and the research team co-led at the Paris Brain Institute by Pr Philippe Fossati and Liane Schmidt, Inserm researcher, coordinated a clinical study involving 26 antidepressant-resistant patients (TRD) and 30 healthy controls.
During the protocol, patients and healthy subjects were first asked to estimate the probability of 40 “negative” events which could occur in their lives (e.g., have a car accident, get cancer, or lose their wallet).
After being informed of the actual occurrence risks in the general population, patients and healthy subjects were again asked to estimate the probability of these events occurring in their lives. The research team was interested in the updating of beliefs after getting information. Results showed that healthy subjects tended to update their initial beliefs more after receiving factual and positive information, which was not the case in the depressed patient population.
In the suite of the study, TRD patients received three administrations of ketamine at a subanesthetic dose (0.5 mg/kg over 40 minutes) in one week. Only four hours after the first administration, patients’ ability to update their beliefs after receiving a positive information was increased. They became less sensitive to negative information and recovered an ability to update their knowledge com parable to that of control subjects.
Moreover, improvement in depressive symptoms after ketamine treatment was associated with these changes in belief updating, suggesting a link between clinical improvement and changes in this cognitive mechanism. “In other words, the more patients’ belief updating ability was increased, the greater the improvement in symptoms was”.
In conclusion, in this study, patients with antidepressant-resistant depression showed a significant decrease in symptoms and became more receptive to “positive” experiences after one week of ketamine treatment.
This work highlights for the first time a cognitive mechanism potentially involved in the early effect of ketamine. It paves the way to new research on antidepressant therapies modulating the mechanisms of belief updating.
Sources
Changing depressive beliefs: An observational study of early Kétamine effects on belief updating biases in treatment-resistant depression
H.Bottemanne & al., Jama Psychiatry, 28 septembre 2022