ALS diagnosis involves a differential diagnosis, meaning that diagnosis occurs after eliminating the possibility of other nervous system conditions.
Differential diagnosis of ALS
ALS diagnosis involves a differential diagnosis, meaning that diagnosis occurs after eliminating the possibility of other nervous system conditions through a normal MRI scan, or confirming the absence of inflammation in the cerebrospinal fluid (which would happen with multiple sclerosis, an autoimmune disease), and if the symptoms do not go away.
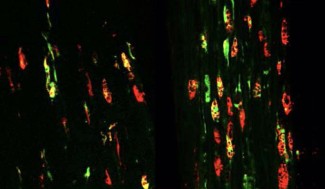
Peripheral neuron degeneration is diagnosed in a clinical examination that identifies muscle atrophy and/or involuntary muscle contractions. An electromyogram can also show a loss of nerve control of certain bulbar muscles and muscles of the cervical and lumbar vertebrae.
Central ALS degeneration is diagnosed by a clinical examination revealing a change in osteotendinous reflexes in atrophied muscle areas.
A genetic study to look for a mutation is only offered for familial forms of the disease (where there have been at least two familial cases, regardless of degree of kinship).
Management of Charcot’s disease
There is currently no cure for ALS.Riluzole is the only drug approved for managing the progression of Charcot’s disease. Multidisciplinary care of patients aims to reduce and relieve symptoms.
This care must be coordinated, evolutive, and adapted to the patient’s stage of disease by different practitioners, including physiotherapists, occupational therapists, speech therapists, nurses, healthcare workers, homecare assistants, mental health support workers, psychologists, dieticians, and other caregivers (family, volunteers). Setting up specialist centers and care networks helps to establish this comprehensive care according to the needs of patients.
When the respiratory muscles are impaired, non-invasive ventilation helps to support declining respiratory function.
At Paris Brain Institute
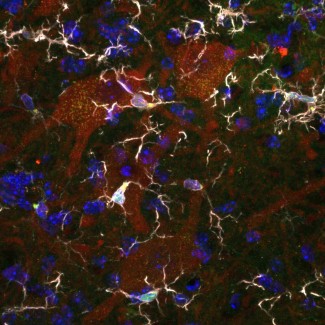
Dr François Salachas, a neurologist who works within Séverine Boillée’s team at Paris Brain Institute, is coordinator of the ALS specialist center at Pitié Salpetrière hospital, while Dr Maria del Mar Amador, a neurologist also on Séverine Boillée’s team at Paris Brain Institute, is the lead ALS genetic counseling researcher at Pitié Salpetrière.
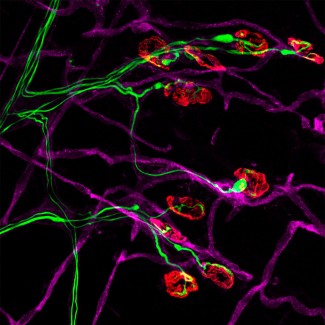
Françoise Piguet, who works in Nathalie Cartier’s team at Paris Brain Institute, is leading an ALS gene and cell therapy project to research ALS treatments. The team is looking at experimental models to optimize the distribution of drug genes and to evaluate the safety and efficacy of these approaches before beginning therapeutic trials.
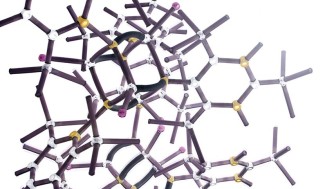
Anti-sense therapy being tested in ALS
There are many promising therapeutic innovations based on antisense oligonucleotide technology – fragments of genetic material capable of binding to messenger RNA, targeting the expression of certain proteins in the central nervous system. After encouraging results in amyotrophic lateral sclerosis (ALS) linked to SOD1 mutations, a new trial (Atlas study) is underway in asymptomatic subjects at risk of developing the disease because they carry this SOD1 genetic mutation. The subjects will be monitored and treated as part of the therapeutic trial as soon as any early signs of the disease emerge.