Two therapeutic approaches are effective in most cases in treating obsessive-compulsive disorder (OCD).
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is based on teaching patients to identify and understand the mechanisms of their disorders and gradually change their behaviors and thought patterns.
Exposure and Prevention Treatment
Exposure and prevention treatment involves exposing patients to situations or people that usually trigger their obsessions while preventing them from performing their compulsive rituals.
For example, a patient obsessed with the risk of contamination and whose ritual involves excessive hand washing may be asked to touch an object he or she considers “dirty,” such as a door handle, without immediately washing their hands.
This repeated methodology enables a habituation mechanism that gradually reduces the anxiety triggered by exposure.
Patients who successfully master this technique can use it on their own outside therapy sessions.
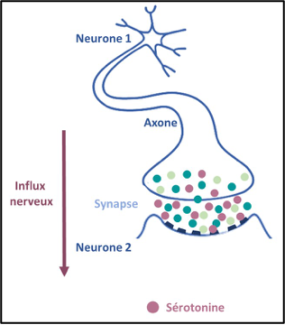
However, some patients who do not respond to this therapy are placed on medication, usually antidepressants to reduce anxiety. These treatments act on serotonin, a molecule that enables communication between neurons via nerve impulses, known as a neurotransmitter.
These treatments for OCD work by increasing serotonin levels in the synapse (the gap between two neurons), mimicking repeated stimulation of the postsynaptic neuron, which reduces anxiety.
At present, a combination of cognitive therapy and medication appears to be an effective approach.
However, 20% of patients with OCD do not respond to these therapies and require alternative treatment involving innovative therapeutic solutions.
Transcranial Magnetic Stimulation
Transcranial magnetic stimulation, used for over 10 years in the treatment of depression, is showing positive preliminary results in OCD. This technique involves using a magnetic field to modify the electrical activity (nerve impulses) of brain neurons.
Deep Brain Stimulation
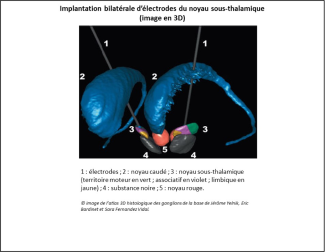
Deep brain stimulation, performed using electrodes implanted in specific regions of the brain that deliver permanent electrical stimulation to neurons in highly targeted areas of the brain, may also be an alternative to conventional treatments.
In 2008, in a prospective, randomized, double-blind study, the team led by Prof. Luc Mallet, psychiatrist and researcher at Paris Brain Institute, demonstrated the safety and efficacy of deep brain stimulation in the treatment of severe and resistant OCD. This study found that after three months of stimulation, more than a quarter of symptoms disappeared in over a third of patients treated.
More than a dozen patients with severe and resistant OCD have now been given implants.