A study by researchers and clinicians from the Paris Brain Institute (Inserm/CNRS/Sorbonne University) and AP-HP (Henri Mondor and Pitié-Salpêtrière Hospitals) confirms the beneficial effect of deep brain stimulation on several brain structures in severe obsessive-compulsive disorders that are resistant to drug treatment. The results are published in the journal Biological Psychiatry.
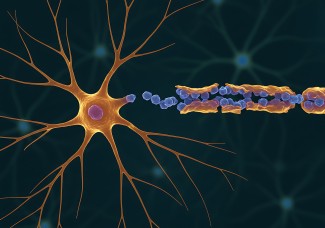
For more than 10 years, deep brain stimulation has been a source of hope for the treatment of obsessive compulsive disorders (OCD), considered one of the most disabling disorders by the WHO. OCD is associated with more years of lost years due to disability than multiple sclerosis and Parkinson's disease combined. It manifests itself in 2 main categories of symptoms: obsessions in the form of thoughts, images with unpleasant content that are involuntarily imposed on the subject. These obsessions generate major anxiety and require the person to perform repeated behaviors and rituals to try to calm these distressing ideas.
Cognitive-behavioural psychotherapy (CBT) and/or serotonergic antidepressants prescribed in high doses to achieve an anti-OCD effect, improve the symptoms of two-thirds of patients. For the remaining third, therapeutic strategies involve complex combinations of treatments, and for a part of them, deep brain stimulation (DBS) represents a real therapeutic perspective.
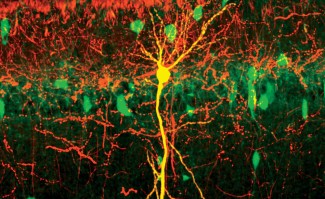
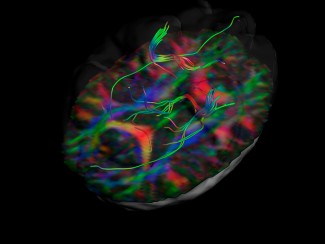
In a new study, published in the journal Biological Psychiatry, researchers and clinicians from the Paris Brain Institute analyzed the effects of DBS on three brain structures, the subthalamic nucleus, the accumbens nucleus and the caudate nucleus, in 8 patients with severe OCD resistant to all available treatments. This is the first study comparing the effect of DBS on three distinct targets in the brain in the same patients.
Their results show an almost equivalent reduction in symptoms regardless of the structure stimulated after 3 months of stimulation, but the majority of patients expressed a subjective preference for the stimulation of a region of the subthalamic nucleus, without knowing that it was this structure that was targeted. They also highlight the possibility of identifying early predictors of response to long-term subthalamic nucleus stimulation.
"Consistent with our previous results*, we also observed a significant improvement of symptoms in longer-term in 3 patients responding to subthalamic nucleus stimulation and a partial response in another 3 patients. This suggests that the most beneficial effects of DBS may be delayed and that this should be taken into account in patient follow-up. The "blinded" choice of patients for this target also shows the interest in taking into account clinical dimensions that go beyond the usual quantitative clinical evaluations to assess a therapeutic effect. "explains Luc Mallet, Professor of Psychiatry at the University of Paris Est Créteil and researcher at the Paris Brain Institute.
The present study confirms the benefit of stimulating different deep brain structures in patients with severe obsessive-compulsive disorders that are resistant to other available treatments, underlining the interest of precisely identifying the neural networks underlying these disorders. Research is still needed to identify precise characteristics that predict whether or not patients will respond to deep brain stimulation.
* Mallet, L., Du Montcel, S. T., Clair, A.-H., Arbus, C., Bardinet, E., Baup, N., Chabardès, S., Chéreau, I., Czernecki, V., Fontaine, D., Harika-Germaneau, G., Haynes, W. I., Houeto, J.-L., Jaafari, N., Krack, P., Millet, B., Navarro, S., Polosan, M., Pelissolo, A. and Welter, M.-L. (2019) ‘Long-term effects of subthalamic stimulation in Obsessive-Compulsive Disorder: Follow-up of a randomized controlled trial’, Brain Stimulation, 12(4), 1080-1082.
Sources
https://pubmed.ncbi.nlm.nih.gov/33012521/
Welter ML, Alves Dos Santos JF, Clair AH, Lau B, Diallo HM, Fernandez-Vidal S, Belaid H, Pelissolo A, Domenech P, Karachi C, Mallet L. Biol Psychiatry. 2020 Oct 2