The diagnosis of parkinson’s disease is based on the identification of a parkinsonian syndrome associated with at least two “supporting” criteria.
Diagnosis of Parkinson's Disease
The diagnosis of Parkinson’s disease is made after the elimination of other pathologies that may give the same early symptoms, such as Wilson’s disease in young people, vascular damage or hydrocephalus more rarely.
Parkinson's disease combines parkinsonian syndrome with at least 2 other criteria out of 4:
- Improvement of Parkinsonian Syndrome Disorders with Dopamine Therapy
- An appearance of involuntary abnormal movements (dyskinesia) after many years of dopamine treatment
- A unilateral or asymmetric resting tremor
- A decrease (hyposmia) or even a complete disappearance (anosmia) of the sense of smell.
Patients may also have so-called “non-motor” symptoms, such as intestinal disturbances, apathy and REM sleep disorders.
At Paris Brain Institute
Many recent studies, particularly those conducted by Marie VIDAILHET and Stéphane LEHERICY’s team at Paris Brain Institute, have shown that the "non-motor" symptoms of Parkinson’s disease are early and begin before the motor symptoms. These clinical signs could therefore be very good diagnostic markers or even serve as prognostic markers of disease progression. In the ICEBERG study, the team focused on REM sleep disorders and eye movements.
This study also identified a marker for the progression of dopamine neuron loss visible on MRI, neuromelanin. This protein plays a protective role in neurons by capturing toxic molecules such as iron.
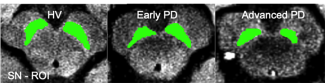
MRI performed by the CENIR imaging platform of Paris Brain Institute. The amount of neuromelanin observed by MRI in the black matter. (Left Healthy individual, centre: early Parkinson's patient, right: long-term patient)
There is a decrease in neuromelanin in patients that increases over time due to degeneration of dopaminergic neurons characteristic of Parkinson’s disease.