We often talk about epilepsy in the plural (epilepsies) because there is such a wide range of types of epileptic seizures and causes. There are many different causes of an epileptic seizure. The main distinction is between structural epilepsies and idiopathic epilepsies.
Structural epilepsy
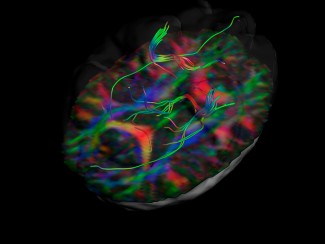
This epilepsy results from a diffuse or local brain injury, resulting in generalized or focal seizures. The injury is most often visible on a brain MRI (and may also be called a symptomatic lesion). It is sometimes not visible (and may also be called a cryptogenic lesion). Lesions can include:
- Hippocampal sclerosis, a scar found in the hippocampus, which is important for memory. This often results in repeated epileptic seizures during fevers in children.
- A brain tumour that affects the cerebral cortex.
- The aftereffects of a stroke, affecting the cerebral cortex.
- A malformation of the cerebral cortex due to a defect in neuronal migration during development, the most common being focal cortical dysplasia.
- The aftereffects of head trauma, often severe.
- The aftereffect of infection such as herpes encephalitis, a parasitic infection
Autoimmune epilepsies
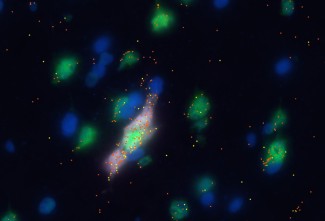
Many autoimmune encephalitis cases are combined with epileptic seizures. These diseases can lead to:
- irregular production of antibodies, which target brain proteins and therefore disrupt neuron function.
- the infiltration into the brain of inflammatory cells such as lymphocytes, which attack neurons.
Identifying these diseases early on allows immunosuppressive drugs to be prescribed – the only way to manage seizures.
The epilepsy unit led by Professor Vincent Navarro at Salpêtrière hospital, a specialist center for rare epilepsies, has substantial expertise in managing these types of epilepsy, which require rapid assessment and sophisticated examinations.
Research work was recently carried out in the ‘Dynamics of Neuronal Networks and Neuronal Excitability’ research term at Paris Brain Institute by Professor Vincent Navarro: the mechanisms of the seizures observed in autoimmune encephalitis linked to an LGI1 antibody were identified. The brief muscle twitches in the arms and the face, characteristic of this disease, were found to be linked to neuron hyperexcitability caused by potassium deficiency (Baudin et al., Prog Neurobiol 2022).
Genetic epilepsy
There are several forms of genetic epilepsy:
- idiopathic epilepsy, believed to be genetic because often another person in the family has epilepsy but no gene mutation has been identified. In idiopathic epilepsy there is no brain injury detectable by MRI. It also has a characteristic age of onset, good response to anti-epileptic treatments and, most often, remission after several years. The electroencephalogram will show typical anomalies. These can be focal or generalized.
- Familial epilepsies caused by mutations identified in genes.
Depending on the mutated gene, brain anomalies may be identified, such as Bourneville’s Tuberous Sclerosis Complex. When the mutated genes encode ion channels (proteins forming tunnels that allow ions such as sodium and potassium to flow in the neuron), no anomalies are detectable by MRI. Mutations in neurotransmitter receptors have also been identified.
‘Situational’ epileptic seizures
Sometimes a seizure occurs in a specific context, even though there is no underlying brain injury or long-term predisposition to recurring seizures. In this situation, the disorder can simply be corrected over time, and long-term anti-epileptic treatment is not needed.
- Excessive and unusual consumption of alcohol, alcohol withdrawal or chronic alcoholism.
- Taking cocaine or amphetamines
- Taking pro-convulsant medicines
- Hypoglycemia (lack of sugar)
- Hypocalcemia (lack of calcium)
- Hyponatremia (lack of sodium)
At Paris Brain Institute
The Genetics and Pathophysiology of Epilepsy team, led by Stéphanie Baulac and Eric Leguern, focuses on the genetic causes of focal epilepsies and cortical development malformations.
In 2013, the team identified the DEPDC5 gene that causes hereditary focal epilepsy and cortical brain malformations (Ishida et al. 2013, Baulac et al. 2015). The team has pioneered the detection of mutations known as somatic mutations, present only in a few brain cells in cortical focal dysplasia. These somatic mutations are de novo mutations that occur during brain development (Baldassari et al. Acta Neuro 2019, Ribierre JCI 2018).
More recently, Stéphanie Baulac’s team provided proof of concept that it is possible to detect the somatic mutations that cause focal epilepsy in connection with a cortical malformation present in a few brain cells, thanks to the DNA circulating in the cerebrospinal fluid (Kim at al. DOI:10.1002/ana.26080) or based on tissue attached to SEEG electrodes used in pre-surgery patient examinations (manuscript currently being prepared). These discoveries open up new pathways for the genetic diagnosis of these conditions.