Jean-Léon Thomas' group (Inserm, Paris Brain institute) just published a 3D mapping of the meningeal lymphatic network and the associated cerebrospinal fluid (CSF) drainage, both in mice and in humans. Beyond the identification of highly conserved structures between the two species, the imaging technique developed for the human study could be valuable for the diagnosis of patients with certain neurological diseases or CSF drainage defects. The results are published in The Journal of Experimental Medicine.
Meningeal lymphatic vessels are necessary for neuroimmune communication and waste removal from the brain.
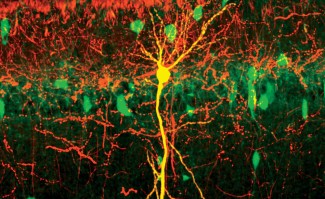
The lymphatic system is a set of vessels, complementary to the blood system, allowing waste elimination, and immune surveillance in organs and tissues. A few years ago, it was demonstrated that this lymphatic network was also present at the edge of the central nervous system, at the level of the meninges - the protective envelopes of the brain and the spinal cord. The anatomical link of the meningeal lymphatic vessels with the lymph nodes of the neck and the peripheral immune system makes them key players in brain immunity control. The meningeal lymphatic vessels are also important for waste removal from the brain, participating in the clearance of interstitial fluid and soluble proteins, as well as the drainage of CSF - the protective fluid surrounding the brain.
The meningeal lymphatic system is affected in many neurological diseases mouse models such as Alzheimer's disease, multiple sclerosis, head trauma and stroke. "Because of its involvement in many diseases, this meningeal lymphatic system has focused a lot of therapeutic interest" explains Laurent Jacob. "However, the anatomy of these vessels, the precise connections they establish with the general lymphatic system and the fluid drainage, never have been explored in whole head approaches, in mice or in humans."
A novel 3D mapping of meningeal lymphatic networks in mice and humans
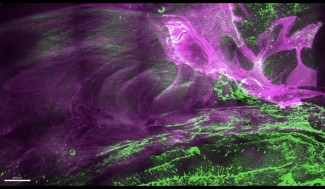
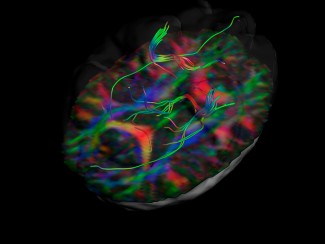
To learn more about the architecture and function of the meningeal lymphatic network, researchers and clinicians from the Paris Brain Institute developed a 3D map of this system. To visualize the lymphatic vessel-wall, two state-of-the-art techniques were used: light-sheet fluorescence microscopy imaging of mouse whole-head, and real time contrast-enhanced magnetic resonance imaging (MRI) in humans. By combining these approaches, the authors rebuilt the entire lymphatic drainage network of the CSF.
A highly conserved architecture between mice and humans
This three-dimensional mapping shows that the architecture of the lymphatic circuits surrounding the brain and connecting to the cervical lymph nodes is very similar between the two species. The mouse model therefore appears to be relevant for preclinical studies in humans targeting meningeal lymphatics system. The 3D imaging also showed that the meningeal lymphatics are in close anatomical relationship with the venous sinuses of the dura mater - collectors of cerebral venous blood. Furthermore, they seem to provide CSF and brain macromolecules transport by very numerous phagocytes present in peri-sinusal spaces. The study thus revealed the existence of a new meningeal lymphatic vascular network around the cavernous sinus, in the anterior part of the skull. It remains to be understood how brain antigens access lymphatic recapture sites in the meninges, and to discover the mechanisms regulating lymphatic-phagocytes interactions and macromolecular transport to the peripheral immune system.
Sexual dimorphism of the meningeal lymphatic network
Quantitative MRI, initiated and performed by Stéphanie Lenck in a dozen patients affected by various meningovascular or neuro-immune diseases, revealed a significantly greater meningeal lymphatic volume in men than in women. Future research will have to explore whether this anatomical data is causally related to the greater predisposition of women to develop neurological diseases such as multiple sclerosis, meningiomas or intracranial hypertension.
Sources
Conserved meningeal lymphatic drainage circuits in mice and humans. Jacob L. et al, Journal of Experimental Medicine. 2022
doi: a venir