A study conducted by Renaud Jardri, Professor at the University of Lille and child psychiatrist at the University Hospital of Lille (Inserm Unit U-1172, University of Lille, University Hospital of Lille - Lille Neuroscience & Cognition), Dr Philippe Domenech at the Brain Institute, and their collaborators, shows that it is possible to predict the occurrence of auditory hallucinations in schizophrenia patients thanks to the combination of functional MRI and artificial intelligence algorithms. These results, published in Biological Psychiatry, pave the way for the development of new neuromodulation and closed-loop neurofeedback therapies to treat these hallucinations.
Functional magnetic resonance imaging (fMRI) capture aims at detecting auditory-verbal hallucinations (AVHs) from continuously recorded brain activity. Establishing efficient capture methods with low computational cost that easily generalize between patients remains a key objective in precision psychiatry. To address this issue, we developed a novel automatized fMRI-capture procedure for AVHs in patients with schizophrenia (SCZ).
We used a previously validated but labor-intensive personalized fMRI-capture method to train a linear classifier using machine learning techniques. We benchmarked the performances of this classifier on 2320 AVH periods versus resting-state periods obtained from SCZ patients with frequent symptoms (n = 23). We characterized patterns of blood oxygen level-dependent activity that were predictive of AVH both within and between subjects. Generalizability was assessed with a second independent sample gathering 2000 AVH labels (n = 34 patients with SCZ), while specificity was tested with a nonclinical control sample performing an auditory imagery task (840 labels, n = 20).
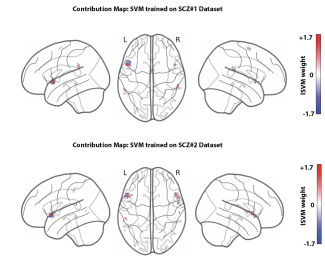
Our between-subject classifier achieved high decoding accuracy (area under the curve = 0.85) and discriminated AVH from rest and verbal imagery. Optimizing the parameters on the first schizophrenia dataset and testing its performance on the second dataset led to an out-of-sample area under the curve of 0.85 (0.88 for the converse test). We showed that AVH detection critically depends on local blood oxygen level-dependent activity patterns within Broca's area.
Our results demonstrate that it is possible to reliably detect AVH states from fMRI blood oxygen level-dependent signals in patients with SCZ using a multivariate decoder without performing complex preprocessing steps. These findings constitute a crucial step toward brain-based treatments for severe drug-resistant hallucinations.