Neurological disorders have been reported in patients with Covid-19. Researchers and clinicians from the Paris Brain Institute and the Hôpital Pitié-Salpêtrière AP-HP have shown the interest of combining different examinations with electroencephalography (EEG), to better identify brain damage, including encephalopathy, in these patients and adapt their management.
SARS-CoV-2 infection is associated in some patients with various neurological symptoms, from loss of smell to consciousness disorders. It is a major challenge to better characterise the brain damage during Covid-19 infection in order to identify the causes and treat patients specifically.
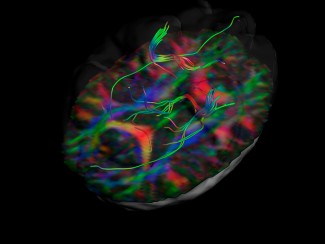
In patients with a neurological form of Covid-19, imaging or biological data (following a lumbar puncture) may suggest a diagnosis of encephalitis. These test results may also be heterogeneous and lack specificity. The combination of these data with EEG, which records the electrical activity of the brain, and clinical evaluation, would make it possible to improve the characterisation of these encephalopathies and better manage patients.
As part of the Covid Neurosciences Cohort project (CoCo Neurosciences), conducted at the Paris Brain Institute (ICM) and the Department of Neurosciences at the Pitié-Salpêtrière Hospital (AP-HP), researchers and clinicians analysed EEG data from 78 patients hospitalised with a Covid-19 infection. The EEG was indicated following significant neurological symptoms such as confusion, epileptic seizures or delayed recovery in intensive care.
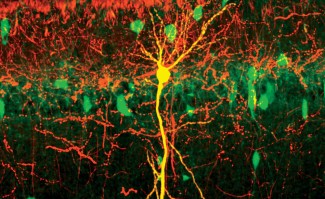
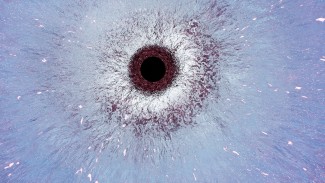
In 69 of these patients, the EEG showed pathological brain electrical activity, such as slow waves, especially in the frontal lobe, periodic repetition activities and epileptic activities. The majority of these patients also had abnormalities on neurological examination, biological tests and brain imaging. Clinicians and researchers sought to explain the causes of these neurological findings for each individual patient using clinical, treatment, biological and imaging data.
Nine patients presented with neurological symptoms, consistent with encephalopathy, with no evidence of any cause or comorbidity other than Covid-19. Compared to the overall cohort, these patients had more frequent abnormal movements, frontal syndrome or brainstem involvement, periodic repetition abnormalities on EEG and white matter involvement on MRI. Their condition was then defined as a Covid-19-associated encephalopathy.
Taken together, these results highlight the value of combining EEG with clinical, biological and imaging data in Covid-19 patients with neurological symptoms. EEG is a valuable tool to distinguish different types of brain damage, including encephalopathies, and thus allow better management of patients.
Sources
Association of Clinical, Biological, and Brain Magnetic Resonance Imaging Findings With Electroencephalographic Findings for Patients With COVID-19.
Lambrecq V*, Hanin A*, Munoz-Musat E, Chougar L, Gassama S, Delorme C, Cousyn L, Borden A, Damiano M, Frazzini V, Huberfeld G, Landgraf F, Nguyen-Michel VH, Pichit P, Sangare A, Chavez M, Morélot-Panzini C, Morawiec E, Raux M, Luyt CE, Rufat P, Galanaud D, Corvol JC, Lubetzki C, Rohaut B, Demeret S, Pyatigorskaya N, Naccache L, Navarro V; Cohort COVID-19 Neurosciences (CoCo Neurosciences) Study Group. JAMA Netw Open. 2021 Mar 1