In intensive care units, some patients who appear unconscious occupy a gray zone in their relationship to the world. To better diagnose them and predict their recovery potential, Dragana Manasova, Jacobo Sitt, and their colleagues have developed an automated tool that integrates multiple modalities for analyzing consciousness. Tested in three European care centers, it could contribute to a more refined and personalized assessment of disorders of consciousness. This work is published in Brain.
After a stroke, traumatic brain injury, or cardiac arrest, some patients sustain severe brain damage and lose consciousness for periods ranging from a few days to several weeks or months. They then may fall along a spectrum of intermediate states between wakefulness and complete loss of consciousness, referred to as disorders of consciousness.
These disorders include, for example, unresponsive wakefulness syndrome (formerly known as the vegetative state), characterized by normal sleep-wake cycles: patients open their eyes and breathe independently but appear unable to interact with their environment. The minimally conscious state, by contrast, shows fleeting signs of awareness: tracking an object with the eyes, reacting to a familiar voice, or making a slight gesture in response to a request.
Helping these patients is extremely difficult. Some certainly understand what is being said to them but cannot express it through voluntary movements—this is known as “cognitive–motor dissociation.”
“There is no clear boundary between normal and abnormal states of consciousness,” explains Dragana Manasova, a former PhD student in the PICNIC Lab at Paris Brain Institute and now a postdoctoral researcher at the Lewis Lab at the Massachusetts Institute of Technology (MIT). “By convention, doctors consider patients to be recovering when they can communicate and manipulate objects. However, patients’ condition can fluctuate considerably, and the timing of improvement remains difficult to predict.”
Uncertainty about patient outcomes complicates clinical care and is a major source of distress for families, underscoring the need to better characterize patients’ states of consciousness and to use the most reliable indicators.
A Wide Range of Indicators
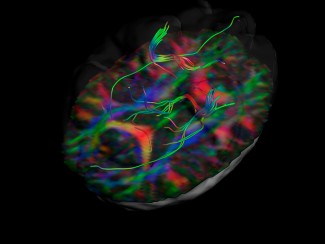
This is the challenge addressed by a multicenter European study coordinated by Jacobo Sitt (Inserm) at Paris Brain Institute, with which Dragana Manasova was involved during her doctoral work. The researchers propose a novel approach: combining six assessment techniques, each capturing a distinct aspect of brain function: high-density electroencephalography (EEG) at rest and during an auditory task, structural and functional MRI, diffusion MRI, and positron emission tomography (PET).
The resulting data are then processed using machine-learning algorithms to make them interpretable. The goal? To determine what each of these techniques reveals about consciousness and how they can be used to improve diagnosis and prognosis.
As part of the European PerBrain consortium, the team recruited nearly 400 patients across France, Germany, and Italy and compared their clinical outcomes with predictions from multimodal analysis.
A Synthetic and Precise Assessment
Their results indicate that combining data from multiple techniques significantly improves model performance: the more modalities available, the more reliable the predictions.
The researchers also show that the modalities that contribute most to diagnosis are not necessarily the same as those that predict patient outcomes.
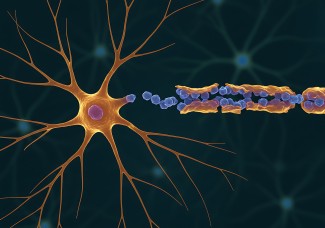
Functional measures of brain activity—metabolic measures from PET or electrical measures from EEG—provide useful information about patients’ current state of consciousness but are less informative about their evolution. Conversely, structural measures, such as diffusion MRI, which analyzes the integrity of brain connections, or conventional MRI, which assesses anatomical integrity, are more relevant for prognosis.
Finally, discrepancies between modalities—for example, between EEG and MRI—are particularly common in patients who ultimately improve. In other words, these divergences, far from being problematic, may actually signal the presence of “islands of consciousness” that are not always captured through clinical observation alone.
Harmonizing patient assessment criteria
The aim of our study was to bring together a wide range of clinical and brain imaging data within a single, coherent analytical framework. By combining these rich and complementary sources of information, we sought to gain a better understanding of complex brain states, as they occur in real-world clinical practice. This work also provides insight into how computational analyses, including artificial intelligence models, can support medical decision-making and help clinicians make more informed choices.
“Now that we have demonstrated the power and usefulness of multimodal analysis in assisting clinicians, we would like to see this tool adopted in expert centers,” explains Jacobo Sitt, co-head of the PICNIC Lab at Paris Brain Institute. “Clinical assessment of patients with disorders of consciousness is not conducted in the same way everywhere; it can vary depending on countries, professional cultures, or access to advanced technologies. Our aim is for all clinicians to share the same reference framework and be able to produce comparable data to advance consciousness research.”
The tool developed by the team is a small, easy-to-use device suitable for clinical settings. It provides a probabilistic and integrative assessment of the patient's condition, giving the medical team full latitude to contextualize and interpret the results.
“This tool does not replace human expertise but offers a way to objectify often ambiguous clinical observations and personalize patient care with a view to achieving the best possible recovery,” the researcher concludes. “It also allows us to better understand the link between brain biology and subjective experience.”
Source
Manasova, D., et al. Multimodal multicenter investigation of diagnostic and prognostic markers in disorders of consciousness. Brain. January 2026. DOI: 10.1093/brain/awaf412.
Funding
This study was funded by Paris Brain Institute America, the European ERAPerMed programme, national research funding agencies in France, Germany and Italy, and the MODELDxConsciousness consortium.
Declaration of interests
Jacobo Sitt is co-founder and shareholder of Neurometers, a company dedicated to the medical use of EEG to quantify brain signatures of consciousness and cognition. The technologies developed by Neurometers are based on tests and protocols developed at Paris Brain Institute and described in this article.
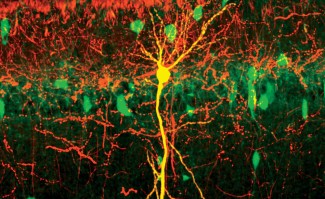
Illustration
Credit: Motion Alchemists, Adobe Stock.

Consciousness, attention, visual perception and language are complex cognitive functions involving different brain areas and neural networks.
Read more