When brain oxygenation is cut off for a prolonged period, the electrical activity of the cerebral cortex is quickly reduced to zero. But that’s not the end of the story… Researchers at Paris Brain Institute, coordinated by Séverine Mahon, have shown that a “wave of death” appearing on the flat electroencephalogram is initiated deep in the cortex. It slowly spreads in this brain region until consciousness is finally extinguished, but it does not always signify permanent death. Indeed, in the event of a successful reoxygenation of the brain, the wave of death is followed by a “wave of resuscitation”, which heralds a slow recovery of brain functions. These findings, published in the journal Neurobiology of Disease, could help researchers determine which populations of neurons are most vulnerable in the event of cardiorespiratory arrest—and ultimately reduce the risk of neurological sequelae.
Death is a difficult concept to define from a neurological point of view. It is not a precise moment that marks the switch from life to death, but a process that lasts several minutes and which, in some cases, can be reversible. In a previous study, researchers from the “Dynamics of Epileptic Networks and Neuronal Excitability” team at Paris Brain Institute showed that after a long period of oxygen deprivation—called anoxia—brain activity undergoes a cascade of successive changes that can now be described precisely.
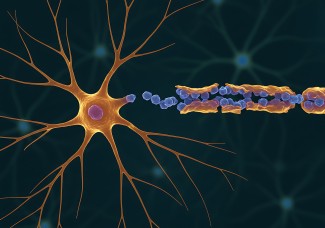
When the brain stops receiving oxygen, its stores of ATP, the cells’ fuel, are rapidly depleted. This causes a disruption in the electrical balance of neurons and a massive release of glutamate, an essential excitatory neurotransmitter in the nervous system. “Neural circuits seem to shut down at first… Then we see a surge in brain activity—specifically an increase in gamma and beta waves,” Séverine Mahon, a researcher in neuroscience, explains. “These waves are usually associated with a conscious experience. In this context, they may be involved in near-death experiences reported by people who have survived cardiorespiratory arrest.”
After that, the activity of the neurons gradually diminishes until a state of perfect electrical silence— corresponding to a flat electroencephalogram—is reached. However, this silence is quickly interrupted by the depolarization of neurons, which takes the form of a high-amplitude wave known as the “wave of death”, which alters the function and structure of the brain.
“This critical event, called anoxic depolarization, induces a state transition in neurons throughout the cortex, rendering them unable to transmit electrical messages. In the absence of intervention, this wave represents the total and definitive cessation of brain activity”
Until now, researchers did not know where the wave of death is initiated in the cortex or whether it propagates homogeneously across all cortical layers. “We already knew that it is possible to reverse the effects of anoxic depolarization if we manage to resuscitate the subject within a specific time window,” the researcher adds. “We still had to understand in which areas of the brain the death wave is likely to do the most damage to preserve brain function as much as possible.”
Following the path of the wave of death
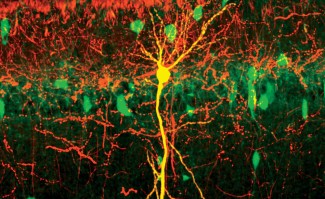
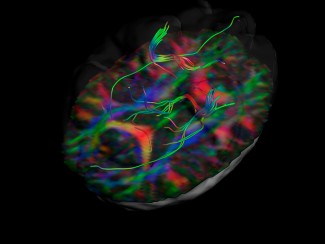
To answer these questions, the researchers used, in rats, measurements of local field potentials and recordings of the electrical activity of individual neurons in different layers of the primary somatosensory cortex—an area that plays a crucial role in body representation and processing of sensory information. They then compared the electrical activity of these different layers before and during anoxic depolarization.
“We noticed that neuronal activity was relatively homogeneous at the onset of brain anoxia. Then, the wave of death appeared in the pyramidal neurons located in layer 5 of the neocortex and propagated in two directions: upwards, i.e. the surface of the brain, and downwards, i.e. the white matter". “We have observed this same dynamic under different experimental conditions and believe it could exist in humans.”
These findings also suggest that the deeper layers of the cortex are the most vulnerable to oxygen deprivation—probably because the pyramidal neurons in layer 5 have exceptionally high energy needs. However, when the researchers reoxygenated the rats’ brains, the cells replenished their ATP reserves, leading to the repolarization of neurons and the restoration of synaptic activity.
“This new study advances our understanding of the neural mechanisms underlying changes in brain activity as death approaches. It is now established that, from a physiological point of view, death is a process that takes its time… and that it is currently impossible to dissociate it rigorously from life. We also know that a flat EEG does not necessarily mean the definitive cessation of brain functions,” Prof. Stéphane Charpier (Sorbonne University), head of the research team, concludes. “We now need to establish the exact conditions under which these functions can be restored and develop neuroprotective drugs to support resuscitation in the event of heart and lung failure.”
FUNDING
This study was funded by Sorbonne University (Emergence-2019), the French National Research Agency and Inserm.
Sources
Carton-Leclercq A. et al. Laminar organization of neocortical activities during systemic anoxia. Neurobiology of disease (2023).
DOI: 10.1016/j.nbd.2023.106345.
Charpier S. Between life and death: the brain twilight zones. Frontiers in Neuroscience (2023).
DOI : 10.3389/fnins.2023.1156368