What if the biological mechanisms that cause multiple sclerosis were triggered years before clinical diagnosis? This is what a team at Paris Brain Institute suggests in a new study published in Neurology. The researchers show that, on a population scale, the frequency of disorders such as depression, constipation, and urinary tract infections is associated with a diagnosis of multiple sclerosis five years later. These results outline a prodromal phase of the disease, but at this stage, they do not allow for the development of an early detection technique.
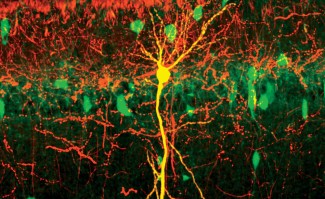
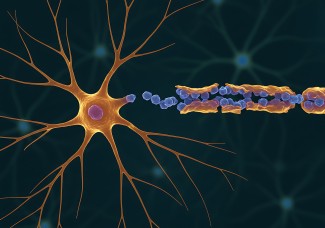
Multiple sclerosis (MS) is a neurological disease in which the immune system attacks myelin, the protective sheath of nerve fibers, which plays a critical role in the spread of nerve impulses between the brain and peripheral organs. In France, 120,000 people are affected by MS, whose management has improved considerably over the last ten years. Unfortunately, there is still no cure to speak of—and no therapeutic solution at all for the 15% of patients with a progressive form.
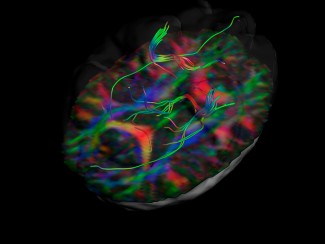
“One of the major difficulties with multiple sclerosis is that we do not observe a strict correspondence between the severity of lesions on nerve fibers and patients’ symptoms. This considerably limits our ability to predict the course of the disease. The challenge today is to detect the disease as early as possible, well before the lesions are visible on MRI, in the hope of delaying the onset of disability.”
Several studies have already suggested that, in some patients, subtle symptoms were present up to ten years before diagnosis. What remained was to quantify this phenomenon at the population scale to rigorously define a “prodromal phase” of multiple sclerosis, i.e., a period during which the disease takes hold discreetly. In addition, a better understanding of the early symptoms of MS could help researchers pinpoint the exact moment when the inflammatory process that causes lesions in the central nervous system begins.
Leveraging massive epidemiological data
To this end, Pr. Céline Louapre, accompanied by Octave Guinebretière and Thomas Nedelac, researchers at Paris Brain Institute as part of the ARAMIS team led by Stanley Durrleman (Inria), compared the health data of 20,174 patients with multiple sclerosis, 54,790 patients without multiple sclerosis, and 37,814 patients affected by two autoimmune diseases which, like MS, mainly affect women and young adults—namely 30,477 patients with Crohn’s disease and 7,337 with lupus.
Using anonymized medical records from the UK’s Health Improvement Network (THIN), the team analyzed the health trajectory of these patients, focusing on the frequency of 113 common symptoms and illnesses over five years before and five years after diagnosis. A similar reference period was used for control patients without autoimmune disease.
The researchers observed that five symptoms were significantly associated with a later diagnosis of multiple sclerosis: depression, sexual disorders, constipation, cystitis, and other urinary tract infections. “This association was sufficiently robust at the statistical level for us to state that these are early clinical warning signs, probably related to damage to the nervous system, in patients who will later be diagnosed with multiple sclerosis,” Prof. Céline Louapre explains. “The overrepresentation of these symptoms persisted and even increased over the five years after diagnosis.”
Shedding light on the trajectory of the disease
However, these five symptoms also appeared in the prodromal phase of lupus and Crohn’s disease, which means they are not specific to MS. Most importantly, they are also widespread in healthy people.
“These signs alone will not be enough to make an early diagnosis, but they will certainly help us better understand the mechanisms of multiple sclerosis—which has many causes—and reconstruct its natural history,” she adds. “Finally, these new data support the idea that the disease begins well before the onset of classic neurological symptoms.”
Only a tiny fraction of people who experience depression, sexual problems, constipation, and urinary tract infections will be diagnosed with an autoimmune disease a few years later. But in populations with a specific risk—in certain familial forms of multiple sclerosis, for example—these signs will help to give early warning and perhaps lead to therapeutic intervention.
Funding
This study was funded by the Joint Programming on neurodegenerative diseases (JPND) of the European Union, the Investments for the Future program, and tANR.
Sources
Guinebretière, O. et al. Association between diseases and symptoms diagnosed in primary care and the subsequent specific risk of multiple sclerosis. Neurology, 6 décembre 2023. DOI : 10.1212/WNL.0000000000207981.