Why does multiple sclerosis progress more rapidly in some patients than in others? Why do some patients with multiple sclerosis succeed in repairing demyelination damage over the course of the disease and others not?
A joint study led by Institut du Cerveau - ICM researchers Violetta Zujovic (INSERM), Isabelle Rebeix (INSERM) and Bertrand Fontaine (AP-HP, UPMC) published in Brain highlighted the key role played by T-cells in myelin regeneration and opened up new opportunities for cell-based therapy.
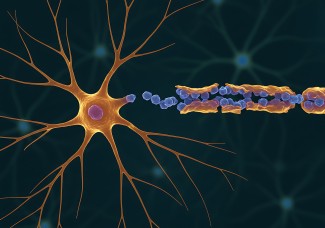
Multiple sclerosis (MS) is an inflammatory disease of the nervous central system leading to a progressive destruction of the myelin sheath surrounding axons, essential for their protection and for the transmission of the nerve impulse. Efficient myelin repair is a key factor in fighting against disease progression. Understanding why and how the illness progresses more or less rapidly in certain patients is essential.
Prior studies have shown that in certain patients, when a lesion appears it is immediately repaired whereas it never repairs itself in other patients. T-cells are the main actors in the inflammatory process through myelin destruction, acting as if myelin was a foreign body. Consequently, Institut du Cerveau - ICM researchers hypothesized that T-cells, key players in inflammation and myelin destruction, may play a part in remyelination success or failure.
To gain a deeper understanding of the process, Institut du Cerveau - ICM researchers (AP-HP, Inserm) grafted T-cells from healthy donors or MS patients in demyelinated spinal cord lesions in mice. Using this new model, they showed that reparative stem/precursor cells are recruited in lesions but do not differentiate into myelin-reparative cells. They highlighted that T-cell activity was enacted through an interaction between macrophages and microglial cells that coordinate repair.
In the case of patients with strong remyelination capacities, T-cells send the appropriate signals to activate repair, leading to cell recruitment and differentiation into myelin-repairing cells. In the case of patients with low remyelination capacities, T-cells do not enable appropriate microglial activation, thereby affecting the entire chain of repair.
Researchers compared T-cell secretion profiles in patients with strong or weak remyelination capabilities, and highlighted 3 molecules associated with proper remyelination and 3 molecules associated with a defect in myelin repair.
Among them, molecule CCL19 is associated with weak remyelination capabilities. Researchers hypothesized that deactivating the molecule would allow microglia and macrophages to reach levels enabling the repair of multiple sclerosis lesions.
Results may direct research towards treatments for other pathologies including amyotrophic lateral sclerosis, Alzheimer’s disease and Parkinson’s disease in which microglia are also essential in lesion repair.