Alzheimer’s disease represents one of the largest remaining unsolved threats to our health. This disease in common with other neurological disorders has been elusive because it is hard to diagnose. Our current ability to diagnose Alzheimer’s disease is equivalent to diagnosing cancer once the disease has metastasized, or equivalent to diagnosing people at risk for heart failures after heart attacks. To develop better treatments of the disease it is first necessary to diagnose it before it is too late, and the symptoms are recognizable as cognitive decline.
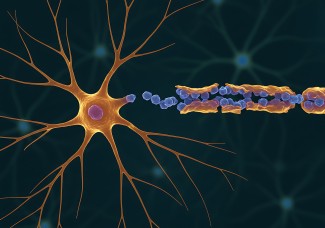
To date it has not proven possible to diagnose Alzheimer’s disease from blood analysis. This is the type of low-cost, simple, biological diagnosis that is necessary for the development of early treatment. Attempts to identify differences in the blood of Alzheimer’s patients from blood of healthy subjects has been frustrated by high levels of individual variability, and because the disease occurs in the brain. The brain is separated from the blood by the Brain-Blood-Barrier (BBB), a barrier that limits the flow of intact proteins from the brain into blood. Short fragments of proteins (peptides) are passed through, but these are difficult to detect with current analytical tools. This means that there is a fundamental technical difficulty associated with using our present tools to diagnose Alzheimer’s disease.
To date diagnostic approaches have been based on the identification of a biomarker, usually a protein, that is associated with the disease. Then an antibody is developed to quantify the biomarker. A new and exciting alternative approach is developing with the use of aptamers instead of antibodies as diagnostic tools. Aptamers are short single stranded fragments of DNA that mimic antibodies in their ability to bind to other molecules. A key difference though is that aptamers are identified by working with large random libraries of sequences in test tubes. These large libraries are characterized by the same advances in DNA sequencing that have enabled the sequencing of the human genome.
We can now characterize how a library of aptamer sequences is responding to all of the differences in blood between a pool of individuals with Alzheimer’s disease and healthy individuals. This publication in Plos One marks the first time that aptamers have been used in this way and thus serves as a benchmark for a whole new approach to the diagnosis of neurological disorders.
This new approach came about as a result of a collaboration between a globally leading aptamer development company, NeoVentures Biotechnology Inc. (Canada) and leading researchers on Alzheimer’s disease at Institut du Cerveau - ICM in Paris including Professor’s Bruno Dubois (Scientific director of "Fondation pour la recherche sur Alzheimer"), Charles Duyckaerts (head of the Laboratoire de Neuropathologie Escourolle at Hopital Pitié salpêtrière and head of the Alzheimer Prion team at Inserm), Harald Hampel (holder of the AXA Research Fund & Sorbonne Université Chair 'Anticiper la Maladie d’Alzheimer') ), Dr. Marie Claude Potier (head of the Alzheimer and Prions team at Institut du Cerveau - ICM) and Magali Dumont (head of the Phenoparc platform at Institut du Cerveau - ICM). This collaboration led to the formation of a French private company, NeoNeuro which has been conducting research for over two years within the Institut du Cerveau - ICM incubator. The company is currently validating the discoveries reported in this paper in human subjects in collaboration with the AIBL cohort (Australia) and the INSIGHT cohort (France).