When a genetically predisposed person is exposed to specific environmental factors, an abnormal inflammatory reaction known as an auto-immune response is triggered by the activation of myelin-reactive immune cells.
These inflammatory phases, which are responsible for multiple sclerosis flare-ups, continue until becoming persistent and chronic inflammation, initiating a cell cascade that causes neuron degeneration and permanent disability.
Multiple sclerosis (MS) is an inflammatory disease of the central nervous system that affects the brain, the spinal cord and the optic nerves, and whose symptoms stem from a reduction in or even an absence of communication between certain regions of the brain, spinal cord and peripheral organs.
The nervous system
Through millions of receptors, the nervous system receives sensory information (from the skin, muscles and sensory organs), via sensory neurons, about changes (stimuli) coming from the internal environment (the body) or from the external environment (the world around us). The central nervous system (brain and spinal cord) assimilates (processes, analyses and interprets) the information it receives: it determines the nature of the information (source, intensity), compares it with its benchmark values and decides on an appropriate response. The central nervous system responds to the assimilated information by instructing motor activity (control) via the motor neurons, such as a muscle contraction. The central nervous system controls and receives information from other organs of the body via the autonomic or vegetative system, i.e. processes over which we have no conscious control, for example our heartbeat.
Neurons
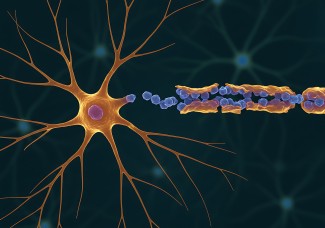
Neurons are the cells that transmit information between the central nervous system and its periphery. They are made up of a cell body, an axon and branched projections called dendrites. Axons emit and receive electrical signals (nerve impulses) which act as the means of sensory and motor communication.
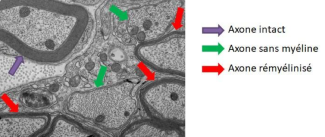
The axons in neurons are protected and nourished by a sheath of lipids – myelin, which acts like an insulator around electrical wires. The myelin also acts as an accelerator of nerve impulses. Myelin makes up the white matter in the brain.
Multiple sclerosis lesions
The lesions or ‘plaques’ we see in the brain or spinal cord in patients during magnetic resonance imaging (MRI) typically feature four components:

- Inflammation: inflammation is the body’s defensive response to external aggression, mediated by immune cells. In multiple sclerosis, the immune reaction is against the body itself; this is called an auto-immune disease. The immune cells attack a component of the central nervous system: myelin
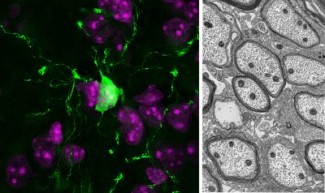
- Demyelination: microscopic observation of a multiple sclerosis lesion. The neurons (cell body and axon) are marked in green, the myelin is marked in red. The disappearance of the protective sheath can be observed in some axon segments.
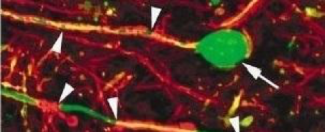
- Neuronal degeneration: without their protective sheath, the neurons deteriorate and die. Looking at this microscopic image, the myelin marked in red has completely disappeared. The axons have retracted and the cell bodies are beginning to die. This is called neuropathy. Myelin attack and neuronal degeneration
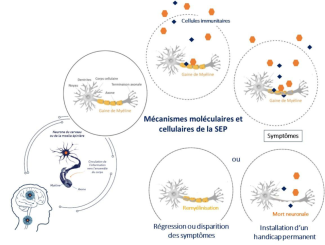

- Repairing Myelin: In some lesions, there is a spontaneous phenomenon of myelin repair. If this occurs at an early stage after the lesion has formed, it prevents neuron death and prevents a disability from developing. Although this is not a rare phenomenon, there is a high level of heterogeneity between patients’ intrinsic ability to repair the lesions caused by multiple sclerosis disease. The nerve impulses disappear in the affected brain regions. Information stops circulating and symptoms emerge.
At Paris Brain Institute
- A study by Beatriz Garcia-Diaz and Anne Baron Van Evercooren (DRE INSERM) at Paris Brain Institute, in the team of Brahim NAIT-OUMESMAR and Violetta ZUJOVIC has recently demonstrated the mechanism that allows Schwann cells to migrate. Schwann cells are the cells that repair the myelin sheath of peripheral neurons in the spinal cord.
- The team of Catherine LUBETZKI and Bruno STANKOFF’s is also leading research projects on demyelination and demyelination mechanisms.
- A collaborative study between the two teams led by Céline Louapre and Violetta Zujovic aims to develop an early assessment tool for the progression of the disability, in order to offer personalized and effective treatment to patients in the early stages of the disease.
Inflammation research
- Several studies by Professor Bruno Stankoff’s team ‘Remyelination in multiple sclerosis: from biology to clinical translation’ have revealed new mechanisms of brain inflammation in multiple sclerosis, thanks to new imaging tools based on a combination of magnetic resonance imaging (MRI) and positron emission tomography (PET).
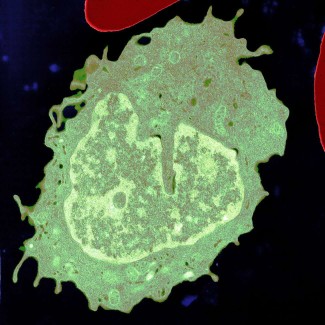
- A collaboration between Violetta Zujovic and Fabrizio De Vico Fallani has identified ‘key’ genes that control the ‘pro-inflammatory’ state of macrophages in multiple sclerosis.
Remyelination research
- In an article published in the European Journal of Neurology, Vito Ricigliano, Benedetta Bodini and their colleagues at Paris Brain Institute demonstrate the protective effect of myelin repair on the tissues surrounding lesions in patients with multiple sclerosis. This discovery highlights the potential of new therapeutic strategies and provides new insights for evaluating the effectiveness of remyelinating drugs being trialed.
- As part of an international consortium, Anne Baron-Van Evercooren and her colleagues have found that the absence of remyelination in some patients with relapsing-remitting multiple sclerosis is not linked to an intrinsic defect in the oligodendrocytes, the brain’s myelinating cells, but instead to the toxic and inflammatory environment of the lesions.
- A study by the ‘Myelin Plasticity and Regeneration’ team, co-led by Brahim Nait-Oumesmar, identified new inhibitors of the kallikrein 6 protein (KLK6) and demonstrated their ability to stimulate myelin production in experimental models.