Multiple sclerosis (MS) is the second leading cause of acquired disability in young adults, after injury. It affects 120,000 people in France today, with 3,000 new cases diagnosed each year. This makes it a major public health issue, since it also affects the active population relatively early in life, with an average onset age of 30.
-
120 Mille personnes touchées en France 2,8 millions dans le monde
-
30 ans âge moyen des patientes et patients
-
75 % des personnes touchées sont des femmes
Multiple sclerosis is an inflammatory disease of the central nervous system (brain, spinal cord and optic nerves). Most patients
present with their first symptoms between the ages of 25 and 35, and a high proportion are women (3 women for every 1 man).
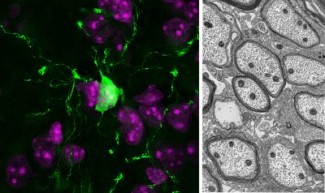
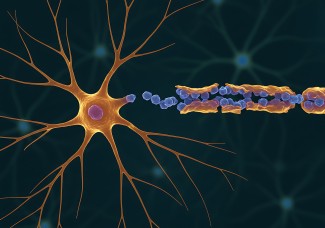
MS suffers typically have lesions known as plaques in which the protective sheath of the neurons, the ‘myelin’, is destroyed, leading to a degeneration of nerve cells known as neurons, with a loss of communication between the brain and its surrounding organs. The myelin provides a protective sheath for the nerve cell extensions (axons).It also supports faster conduction of nerve impulses. This condition is known as an autoimmune disease because, in MS, the immune system, whose role is to protect the body from pathogenic agents (viruses, bacteria), attacks the body itself – in this case the myelin.
Multiple sclerosis (MS) usually evolves in two phases. The first phase typically occurs with relapses of transient symptoms. This is called the remitting phase.
It begins around the age of 30, and accounts for 85% of initial forms. The second phase generally begins 10 to 20 years after disease onset, and is referred to as the progressive phase. In this second phase, the onset of permanent residual symptoms continues, leading to cognitive or motor functional impairment.
Retrouvez la page dédiée à notre vidéo "Comprendre en 2 minutes : la sclérose en plaques (SEP)"
The different forms of multiple sclerosis progression
The two forms of MS can have different variations.
- Relapsing-remitting multiple sclerosis: This is the most common form of MS at early onset of the disease (80 to 85% of cases). In this form of MS, acute phases – or relapses – are experienced, during which patients present with numerous intense symptoms that alternate with periods of complete remission, with no symptoms. The relapses can last from a few days to a month, without any impairment developing between symptomatic phases.
- Secondary progressive multiple sclerosis: In more than half of patients, this phase appears after 5 to 20 years of relapsing-remitting MS. It involves the onset of a permanent and progressive disability.
- Primary progressive multiple sclerosis: These forms of MS affect 10 to 15% of patients from disease onset, and they progress very rapidly. The impairment continues to progress without remission phases. In general, these forms of MS occur in older people, with an average age of around 60.
MS can affect all the functions of the nervous system to varying degrees, depending on the individual: vision, motor skills, balance and coordination, sensations, memory and intellectual capacity.
What causes multiple sclerosis? Is it hereditary?
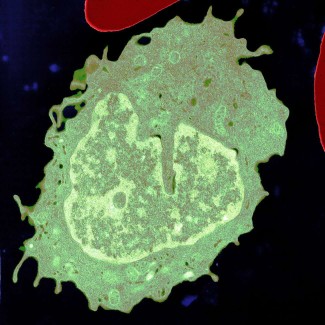
Multiple sclerosis is a multifactorial disease. It occurs in people who are genetically predisposed to it, after exposure to one or more unidentified environmental factors.
There are no hereditary forms of the disease, and a monozygotic twin (identical twin) of an affected person, i.e. a twin with the exact same DNA, only has a 25% risk of developing the disease. This confirms that the disease has a genetic component, but also that it is not hereditary.

Biological mechanisms of multiple sclerosis
Multiple sclerosis is an inflammatory disease of the central nervous system (brain and spinal cord). In MS, an immune attack occurs on a protein, the myelin, which protects neurons and helps to carry nerve impulses.
We refer to MS as an autoimmune disease because the immune system, whose normal role is to protect the body against viruses and bacteria, attacks a part of the body.
The loss of myelin in the lesions typically seen in multiple sclerosis (plaques) makes it impossible for the nerve signals to reach the surrounding organs, especially the muscles. Some patients are able to reform the myelin sheath, especially at the start of the disease. This means that the condition progresses more slowly in these patients, and the onset of impairments is delayed. Current research into therapies is based on this observation, to determine which physiological mechanisms are potentially involved.

Multiple sclerosis diagnosis and symptoms
Multiple sclerosis diagnosis requires an identification of this combination of neurological symptoms with the presence of inflammatory plaques in an MRI scan, to see which respond to spatial dissemination (brain, spinal cord, optic nerve) and temporal dissemination (inflammatory plaques of different ages or that appear over time).


Treatments for multiple sclerosis
There is currently no cure for multiple sclerosis. Therapies aim to reduce inflammatory reaction and therefore slow the progression of impairments. By observing intrinsic individual capacity to repair lesions caused by immune attack, this opens up potential new therapeutic approaches.

Support Paris Brain Institute
Did you like this content and did it answer the questions you were asking? Don't hesitate to support Paris Brain Institute.