Multiple sclerosis diagnosis requires this combination of neurological symptoms with the presence of inflammatory plaques in an MRI scan, to see which have both spatial dissemination (brain, spinal cord, optic nerve) and temporal dissemination (inflammatory plaques of different ages or that appear over time).
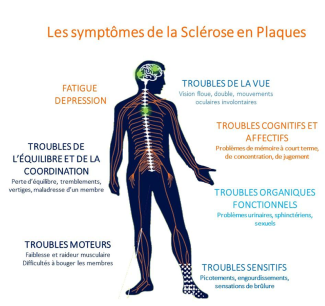
Symptoms of multiple sclerosis
The symptoms are extremely varied according to the area of the brain, spinal cord or optic nerves where the inflammatory attack occurs. They can therefore manifest as:
- sensitivity disorders (pins and needles, tingling, feeling a cold or prickling sensation on the skin, a feeling of tightness or pain)
- muscle paralysis or weakness leading to problems walking
- balance problems
- visual impairment. The disorder results in a loss of visual acuity that can be accompanied by pain around the eye socket, especially when the eye is moving.
In some cases, the starting symptoms may differ between two episodes. For example, one with sensitivity problems in a lower limb, but then a few weeks later problems with vision.
The symptoms of multiple sclerosis (MS) differ greatly from one patient to another. The spread of lesions over time and in different regions of the brain and spinal cord explains why there is so much variation in symptoms in the same patient, as well as between patients.
The most well-known symptoms of the disease are its motor symptoms. Problems with walking, or with moving a lower or upper limb, are all external signs visible to those around the patient. However, although the symptoms of multiple sclerosis can be very debilitating for a person in their everyday life, not all are noticeable and are therefore less well understood and accepted by the patients’ friends and relatives. These symptoms include fatigue and tiring easily, affecting 75 to 95% of patients with MS. This fatigue can be physical as well as mental and can have a considerable impact on patients’ daily lives. Another of the invisible symptoms is cognitive impairment, which presents as problems with attention, concentration, memory, and executive function disorders such as decision-making, planning, organization, etc. Finally, mood or emotional disorders may also be present.
In the first few years of the disease, in more than 80% of cases, the disease progresses as inflammatory flare-ups (recurrent-remitting form). A flare-up typically begins within a few days or months and lasts around 2 to 8 weeks. After several years, some patients develop a secondary progressive form. The time to onset of this form can vary widely between individuals and could depend on individual recovery capacity. The other 20% of patients present with a progressive form from the outset. The progression and time to onset of irreversible disability vary according to each person’s ability to ‘repair’ their brain damage.